Metalloestrogens
Stealth toxins that can play havoc with your hormones.
InterClinical eNews December 2019, Issue 99

Metalloestrogens – Factors influencing Susceptibility
Several metals can act as metalloestogens by binding to the oestrogenic receptor alpha and initiating cellular changes. However, not everyone exposed to toxic metals develops symptoms. (1) Some factors which affect the likelihood of developing symptoms include:
- Timing and duration of exposure – This appears critical. For example in hypogonadal males, correcting the hormone levels after the development of the gonads does not correct the problem due to the absence of adequate numbers of sertoli cells normally formed during the critical perinatal developmental window.
- Level of accumulation and distribution – Within the body metalloestrogens act in a dose-dependent manner.
- Windows of sensitivity – Critical periods of susceptibility where individuals are more prone to the toxic effects of metal excess have been identified as: pre-birth, adolescence, pregnancy and menopause.
- Genetic polymorphisms – These can predispose individuals to bio-accumulate heavy metals especially those with a genetic variation in the metal-carrying protein metallothionein 2A gene. (2,3)
Metalloestrogens – Modes of Action
The actions of metalloestrogens are many and varied with some metals exerting direct effects upon the oestrogen receptors themselves. Others act indirectly by modulating oestrogen receptors in various ways. And a third group cause toxicity by forming reactive oxygen species or by inducing oxygen species. These free radicals are cytotoxic and interfere with hormonal health and reproduction. The key features of this pathway disruption are depicted in Fig. One below. (2)

Cadmium
There is increasing epidemiological evidence linking exposure to cadmium with a heightened risk of women developing breast cancer. Three very large US epidemiological studies, comparing occupation to incidence/or death rates from breast cancer, showed workers from cadmium-based industries were a third more likely to contract breast cancer. In another large, within population, prospective cohort study, higher long-term dietary intake of cadmium was associated with a nearly three-fold increased risk of endometrial cancer in postmenopausal women. (2)
Two recent meta-analysis both concluded that most of the epidemiological, in vivo, and in vitro studies strongly support the link between increased cadmium exposure and breast cancer development. (2,4,5,6) Cadmium also mimics oestrogen-driven cell proliferation and prolactin secretion from the anterior pituitary cells. (7)
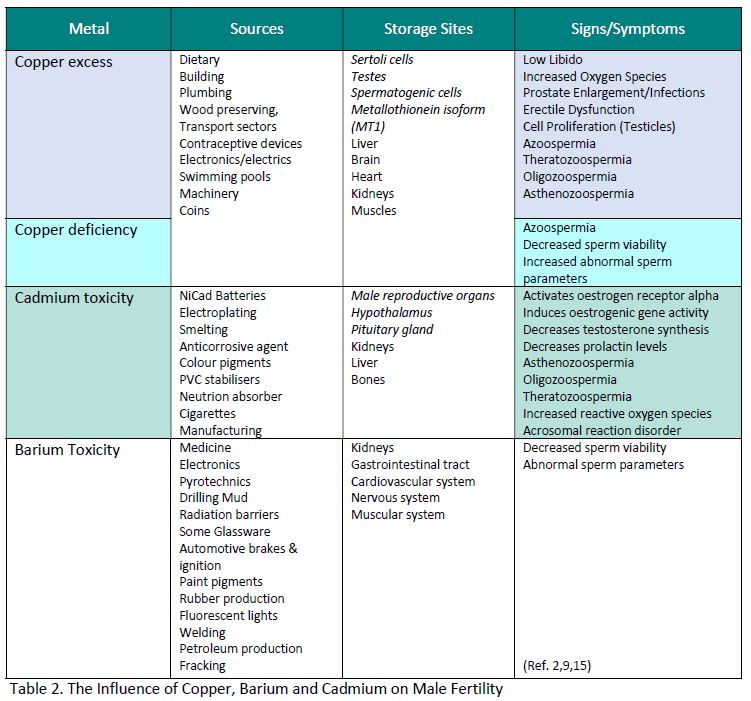
In males, cadmium activates the oestrogen receptor alpha and induces oestrogenic gene activity. It has been shown to decrease testosterone, the main male hormone. It is also associated with a number of pathological changes to sperm quality and viability and with hampering the union of egg and sperm union. (2)
Copper
Copper is a metal essential for normal foetal development. Its normal physiological function is to help induce ovulation indirectly by catalysing the hydroxylation of dopamine to noradrenaline. Noradrenaline is an essential neurotransmitter involved in the secretion of gonadotrophin releasing hormone, which in turn, is involved in the release of luteinising hormone and follicle stimulating hormone from the anterior pituitary. Together these hormones help initiate and maintain ovum health. (2)
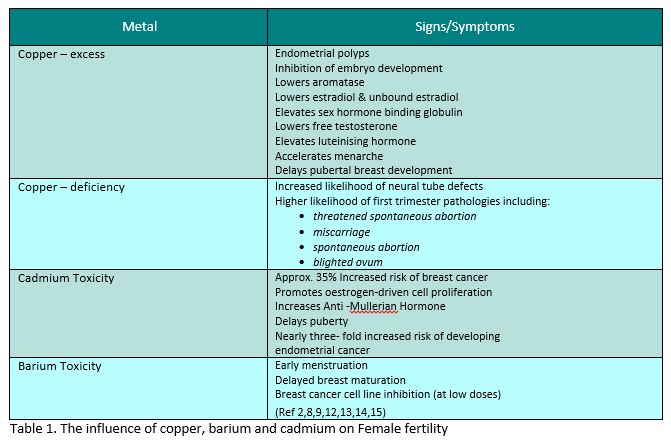
Due to its importance, the human foetus stores, weight for weight, up to 10 times more copper than adults. A deficiency during pregnancy has been shown to affect foetal development detrimentally with an increased chance of neural tube defects and a significantly higher likelihood of first trimester pathologies, see Table 1 for details. (2,8,9) Whereas copper excess has been associated with a dose-dependent inhibition of embryo development. (2)
Unfortunately, exogenous copper, has also been shown to act as a metalloestrogen capable of directly inducing ovulation (in experimental models). In men, copper exposure is associated with a plethora of spermatological abnormalities, some prostate disorders, and erectile dysfunction. Copper excess can affect male sexual health, fertility and procreation ability. It has also been linked with increased risk of testicular cancer. Together these findings suggest that both, too little, or too much copper can be problematic for male and female hormonal health as well as foetal wellbeing, as outlined in Table 1 & 2 below. (2)
Barium
Scoring highly on the list of oestrogenicity of metals is barium, however only very limited research into its effects on hormonal health is available to date. At low doses it may exert beneficial anti-tumour effects as shown in the following study. Barium chloride exhibited dose-dependent antitumor effects against human MCF-7 breast cancer cells co-cultured with MN cells, thereby offering a possible therapeutic alternative for treating this disease provided they are administered at very low concentrations. (10)
However, caution is advised in interpreting these results. In another study of peripubertal girls, high concentrations of barium were associated with being at a higher pubic hair Tanner stage and menarche at 8-13, but lower odds of progressing to the next stage of breast development at 14 – 18 years. The researchers note a possible impact of barium toxicity on pubertal timing with adverse health outcomes for adolescent girls. (11) In males, barium has also been shown to affect sperm parameters deleteriously.
Heavy Metal Impact on Female Fertility
Heavy Metals Impact on Male Fertility
Metallic Nanoparticles
Apart from traditional sources of metal burden, there is early evidence to suggest metallic nanoparticles may be toxic, due to their bypassing normal biological barriers within the body. Copper has been shown to have estrogenic effect, but it is uncertain whether other common metallic nanoparticles, such as silver, zinc and titanium, produce similar actions. Additionally, some metals have been shown to increase production of reactive oxygen species and to cause DNA fragmentation. The body uses several carrier molecules and numerous biological gates to prevent the accumulation of metals within tissues, bypassing these carrier systems may inadvertently predispose the body to toxicological issues. (16)
It has been shown that metalloestrogens including cadmium, copper and barium, can directly impact oestrogen activity within the body. Metalloestrogens are also associated with an increased likelihood of pathological changes to hormonal and reproductive health and impaired antioxidant status. In patients with hormonal or reproductive health concerns it may be prudent to test for the presence of heavy metals. Once identified these metals can be brought back into normal range by the use of antagonistic minerals and vitamins which in turn, help to restore hormonal health.
InterClinical Comment
Hair Tissue Mineral Analysis is a safe, reliable, non-invasive, easy pathology test to help determine your client’s body burden of heavy metals including cadmium, copper and barium.
A test for heavy metals will provide you with a wealth of information. Knowing the ratio of essential nutrient minerals against the body burden of toxic elements helps provide the knowledge needed for a targeted treatment plan. With this knowledge you can confidently prescribe the right supplements to both detoxify and protect against the harmful effects of heavy metals.
References
- Lappano R, Malaguarnera R, Belfiore A, Maggiolini M. Recent advances on the stimulatory effects of metals in breast cancer. Molecular and cellular endocrinology. 2017 Dec 5;457:49-56.
- Jurkowska K, Kratz EM, Sawicka E, Piwowar A. The impact of metalloestrogens on the physiology of male reproductive health as a current problem of the xxi century. JPP. 2019(3):02.
- Joneidi Z, Montazavi Y. Roointan A. Charhardouli B. Rostami S. The impact of genetic factors on metabolism of heavy metals: genetic predisposition? Biomed. Pharmacother. 2019:113:108642
- Aquino NB, Sevigny MB, Sabangan J, Louie MC. The role of cadmium and nickel in estrogen receptor signaling and breast cancer: metalloestrogens or not?. Journal of Environmental Science and Health, Part C. 2012 Jul 1;30(3):189-224.
- Byrne C, Divekar SD, Storchan GB, Parodi DA, Martin MB. Metals and breast cancer. Journal of mammary gland biology and neoplasia. 2013 Mar 1;18(1): 63-73.
- Larsson SC, Orsini N, Wolk A. Urinary cadmium concentration and risk of breast cancer: a systematic review and dose-response meta-analysis. American journal of epidemiology. 2015 Aug 6;182(5):375-80.
- Ronchetti SA, Miler EA, Duvilanski BH, Cabilla JP. Cadmium mimics estrogen-driven cell proliferation and prolactin secretion from anterior pituitary cells. PLoS One. 2013 Nov 13;8(11):e81101.
- Alebic-Juretic A, Frkovic A. Plasma copper concentrations in pathological pregnancies. Journal of Trace Elements in Medicine and Biology. 2005 Dec 2;19(2-3):191-4.
- Roychoudhury S, Nath S, Massanyi P, Stawarz R, Kacaniova M, Kolesarova A. Copper-induced changes in reproductive functions: in vivo and in vitro effects. Physiological research. 2016 Feb 1;65(1).
- Da Silva FH, Ribeiro AA, Deluque AL, Cotrim AC, de Marchi PG, França EL, Honorio-França AC. Effects of barium chloride adsorbed to polyethylene glycol (PEG) microspheres on co-culture of human blood mononuclear cell and breast cancer cell lines (MCF-7). Immunopharmacology and immunotoxicology. 2018 Jan 2;40(1):18-24
- Ashrap P, Sánchez BN, Téllez-Rojo MM, Basu N, Tamayo-Ortiz M, Peterson KE, Meeker JD, Watkins DJ. In utero and peripubertal metals exposure in relation to reproductive hormones and sexual maturation and progression among girls in Mexico City. Environmental research. 2019 Oct 1;177:108630.
- Yilmaz BK, Evliyaoglu O, Yorganci A, Ozyer S, Ustin YE. Serum concentrations of heavy metals in women with endometrial polyps. J Obs & Gyn 2019:1-5
- Christensen PS, Bonde JP, Bungum L, Giwercman A, Toft G, Jönsson BA, Specht IO. Environmental cadmium and lead exposure and anti-Müllerian hormone in pregnant women. Reproductive Toxicology. 2016 Jun 1;61:114-9.
- De Craemer S, Croes K, van Larebeke N, De Henauw S, Schoeters G, Govarts E, Loots I, Nawrot T, Nelen V, Den Hond E, Bruckers L.
- Kumar S, Sharma A. Cadmium toxicity: effects on human reproduction and fertility. Reviews on environmental health. 2019 May 27.
- Wallace DR. Nanotoxicology and metalloestrogens: Possible involvement in breast cancer. Toxics. 2015 Dec;3(4):390-413.
Copyright InterClinical Laboratories 2019, 2020