Immune System Patterns in Hair Tissue Mineral Analysis
InterClinical eNews March 2020 Special Edition
The wonder of our immune system
Our immune system is miraculous and complex. Research into how it functions reveals a sophisticated security system that constantly scans the body to identify and remove any threat to our well being.
Receptors associated with the immune system are concerned with interrogating the environment for evidence of danger, infection or abnormal cell death. They are also present inside the cell where they play an important role, acting to detect evidence of infection.
Organisms such as viruses can spend most of their life hidden in the complicated cytoplasm of the cell, making them difficult to recognize from the outside. Infections reproduce much more rapidly than their hosts and can change their appearance allowing them to evade recognition. An effective immune system must adapt to these constant changes.1
Our immune system can harm
A pathogen that has penetrated the body’s defenses and established itself within or between cells can only be eliminated by killing. This is a dangerous business, and when the immune system is battling with an infection, it may put the life of the host at risk.
For instance when a common cold virus has hijacked a cell to replicate itself, the cell is not rehabilitated, it is destroyed by killer cells. There is growing evidence that cells are damaged not directly by replicating viruses but by a specific immune response that produces the symptoms of disease.2 The immune response must take a middle path that is between too much destruction and not enough.1
One factor that that can limit damage is interleukin 10 (IL-10). IL-10 is an anti-inflammatory cytokine that may be of particular importance to constrain the severity of inflammatory reactions caused by chronic infections. It corrects the impairment of epithelial barrier function and restores small intestine homeostasis. And in a recent study IL-10 production by virus specific effector cells during the acute response to influenza virus was shown to be responsible for minimising the severity of pulmonary lesions in mice.3
However, IL-10 production by intestinal resident macrophages is impaired by nutritional deprivation.4 Inadequate nutrition impairs the functioning of the immune system. This can result in, not only increased susceptibility to infection, but an increased severity in cell damage as the immune system responds to invaders.5
When nutritional status is compromised due to infections, malabsorption and chronic disease, the body’s free radical quenching capabilities may be reduced considerably, even during a normal immune response. The immune response can be affected not only by individual nutritional deficiency, but also by nutritional imbalances.6
The two branches of our immune system and how they work
The primary organs of the immune system include the thymus and bone marrow. The thymus is involved in hormone production and the development of immunocompetent T-Cells. Whereas the bone marrow produces the stem cells that differentiate into lymphocytes, erythrocytes, granulocytes and megakaryocytes.
The secondary organs of the immune system include the lymph nodes and tonsils which are responsible for prevention and spread of infection; the spleen, which primarily produces B-Cells and T-Cells; and finally the Peyer’s Patches of the gut, which are responsible for T-Cell production.7
Our immune system can be classified into two different branches, the cellular and humoral.
The cellular immune system
The cellular immune system is mediated by antigen-specific T-Cells which are produced in the bone marrow and matured in the thymus. These T-Cells are the body’s defense against viruses, fungi, and intracellular organisms. They can be found in blood as well as lymphoid tissue. T-Cells activate the B-Cells of the humoral immune system.6
The humoral immune system
The name humoral immune system, comes from its involvement in substances found in the humors or body fluids. It protects the intracellular spaces where antibodies, produced by B-Cells, destroy extracellular microorganisms, and prevent bacterial infection.6
These two branches, the cellular and humoral, function together in a normal healthy individual. However, one group can become dominant and become antagonistic to the other. This causes the immune system to lose its synergistic relationship and become unbalanced causing the dominant side of the immune response to suppress the other.
For example, the humoral immune system can act to the detriment of the host, and block the activity of the cellular immune system in its attempt to destroy abnormal cells. On the other hand when the cellular immune response dominates there is a suppression of the humoral immune system.6
Let’s examine nutritional deficiency and its impact on the two branches of the immune system.
Endocrine and immune system interactions
Recently, it has come to light that while the immune system interacts directly within brain regions that regulate autonomic function, the autonomic nervous system innervates organs that contain immune cells, such as the spleen and bone marrow. Indeed, effects on immune cells of both the parasympathetic and the sympathetic nervous system have been described.8
Our endocrine system is intimately involved with our immune system. Hormones and neurotransmitters are specific modulators of cells and of the immune system by fine tuning their activation. Hormones are able to regulate the recruitment of immune cells to an inflammatory site, and have an impact on the intracellular signaling cascades that follow after tissue injury.13
The sympathetic and parasympathetic influence
Generally speaking the sympathetic nervous system speeds up the activity of the body, while the parasympathetic branch slows it down. They have an effect on the rate of organ function, enzyme activity, immunity, and hormone release. The parasympathetic and sympathetic branches oppose each other and work in concert with the endocrine glands of the body.7
Endocrine system according to stimulating or sedating effects
| Sympathetic Endocrine Glands | Parasympathetic Endocrine Glands |
| Hypothalamus (Medial portion) Anterior Pituitary Adrenal Cortex (Catabolic) Adrenal Medulla Thyroid Ovaries (Progesterone) | Hypothalamus (Lateral portion) Posterior Pituitary Adrenal Cortex (Anabolic) Pancreas (Endocrine) Parathyroid Ovaries (Estrogen) |
7
Parathyroid and the cellular immune response
Both B and T-Cells contain receptors for parathyroid hormone (PTH). This indicates that they are probably target organs for the action this hormone. PTH affects T-Cell function and plays a role in the commencement of abnormalities in cellular immunity. The action of PTH on T-Cells in culture is dependent on the presence of calcium and is accompanied by a rise in cytosolic calcium. 10
Excessive calcium increases viral proliferation and is generally found in the presence of an increase in thymus response. Viral infections produce a sedative effect that slows down the metabolic rate. Both calcium and magnesium have a sedating influence and are classified as parasympathetic minerals, with a predisposition to viral manifestation and parathyroid dominance.6
Sympathetic and the humoral immune response
Bacterial infections produce a stimulatory response and increase the metabolic rate.7 When an antigen enters the body, local activation of immune cells leads to the release of pro-inflammatory mediators, if these are strong enough it signals to the brain resulting in the activation of the sympathetic nervous system.11
The sympathetic endocrine group can be referred to as the stress glands. They are activated by stress and in turn raise the metabolic rate. In a sympathetic dominant individual sodium, potassium and phosphorus can build up due to a change in intestinal absorption and reabsorption by the kidney.7

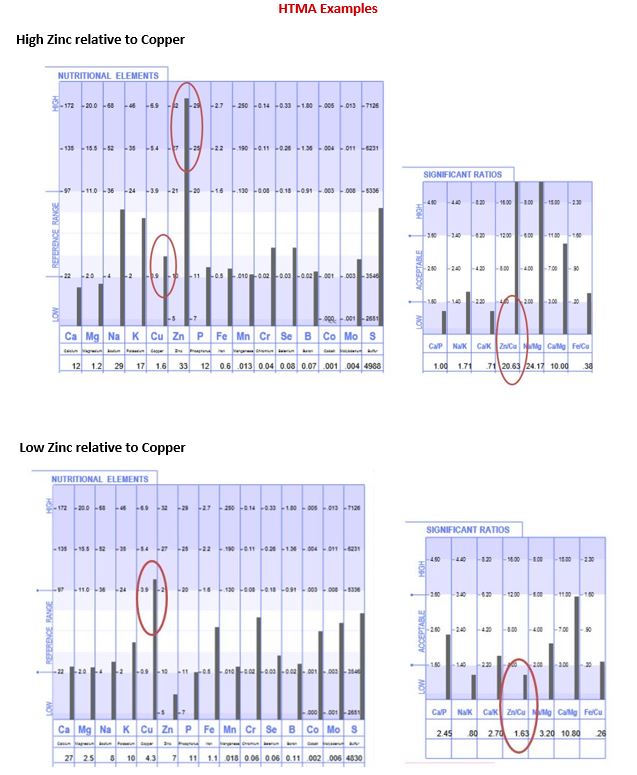
Hair Tissue Mineral Analysis and nutrients for the parasympathetic response
As stated previously the parasympathetic dominant individual will tend toward a cellular immune or thymus mediated response. In its extreme state it can result in the inability to initiate a humoral or bacterial immune response. On a Hair Tissue Mineral Analysis (HTMA) report this metabolic type will display an elevation of calcium and magnesium relative to lower phosphorus, sodium and potassium. This type can often show lowered zinc levels, which is associated with increased viral susceptibility, and elevated hair tissue levels of copper.7
Elevated calcium concentrations can be viral-inducing. Nutrients synergistic to calcium can be seen as viral-activating agents. These include vitamin D and copper. However, any substance that contributes to the reduction in tissue calcium should aid in viral resistance. These include vitamin C, vitamin A, panthothenic acid, niacin, vitamin B6, zinc, magnesium, iron and phosphorus.7
Hair Tissue Mineral Analysis and nutrients for the sympathetic response
The humoral response is associated with resistance to bacteria and thymus suppression. Low hair tissue copper, calcium and magnesium relative to elevated sodium and potassium is typically found in an individual with a sympathetic dominant response.
In bacterial infections, one of the first things to occur is the withholding of nutrients to prevent bacterial outgrowth.12 The most significant form of nutritional immunity involves the body taking iron out of circulation to reduce its availability to bacteria which need iron to proliferate. During bacterial infections a hair tissue study shows high levels of iron, however serum iron will be low. This will be accompanied by a mobilization of copper into the blood to combat the infection. Therefore, hair tissue would show a marked reduction in copper.7
Nutrients that support the individual with a humoral immune response can help to sedate the sympathetic metabolic process and balance the immune response. These are calcium, magnesium, zinc, copper, chromium, vitamin B2, vitamin B12 and vitamin D.7
InterClinical Comment
Understanding the two sides of the immune system, the cellular and humoral, can provide a practitioner with a wealth of information. Hair Tissue Mineral Analysis (HTMA) can help unravel the puzzle of how to support a patient during times of chronic viral or bacterial infection. Identifying your patients nutrient mineral deficiencies and excesses, combined with the knowledge of significant mineral ratio imbalances will help provide, an otherwise very difficult to determine, individualised program of nutritional supplementation to rebalance an out of kilter immune system. For more information about InterClinical Laboratories HTMA testing, visit here.
For more information, please open the link below to access an article written by Dr. David Watts in 1994 titled THE IMMUNE SYSTEM AND HAIR TISSUE MINERAL PATTERNS Nutritional, Neuro-Endocrine Immunology (David L. Watts, Ph.D., Director of Research TEI Lab) https://www.traceelements.com/Docs/News%20March-April%2094.pdf
REFERENCES
1. Nicholson, L. B. (2016). The immune system. Essays In Biochemistry, 60(3), 275–301. doi:10.1042/ebc20160017
2. Notkins, A. L., Koprowski, H. (1973) How the Immune Response to a Virus Can Cause Disease. Scientific American 228(1) 22-31.
3. Rouse, B. T., & Sehrawat, S. (2010). Immunity and immunopathology to viruses: what decides the outcome? Nature Reviews Immunology, 10(7), 514–526. doi:10.1038/nri2802
4. Ochi, T., Feng, Y., Kitamoto, S., Nagao-Kitamoto, H., Kuffa, P., Atarashi, K., … Kamada, N. (2016). Diet-dependent, microbiota-independent regulation of IL-10-producing lamina propria macrophages in the small intestine. Scientific Reports, 6(1). doi:10.1038/srep27634
5. Beck, M. A., & Levander, O. A. (2000). Host Nutritional Status and Its Effect on a Viral Pathogen. The Journal of Infectious Diseases, 182(s1), S93–S96. doi:10.1086/315918
6. Watts D. (1994) The Immune System and Hair Tissue Mineral Analysis. Nutritional, Neuro-Endocrine Immunology. Newsletter.
7. Watts DL. Trace Elements and Other Essential Nutrients. 5th Edn. Writers BLOCK, USA.; 1995.
8. Rosas‐Ballina M, Olofsson PS, Ochani M, Valdés‐Ferrer SI, Levine YA, Reardon C, Tusche MW, Pavlov VA, Andersson U, Chavan S, Mak TW & Tracey KJ (2011). Acetylcholine‐synthesizing T cells relay neural signals in a vagus nerve circuit. Science 334, 98–101.
9. Carvalho, L. A., Gerdes, J. M., Strell, C., Wallace, G. R., & Martins, J. O. (2015). Interplay between the Endocrine System and Immune Cells. BioMed Research International, 2015, 1–2. doi:10.1155/2015/986742
10. Shurtz-Swirski, R., Shkolnik, T., & Shasha, S. M. (1995). Parathyroid Hormone and the Cellular Immune System. Nephron, 70(1), 21–24. doi:10.1159/000188538
11. Pongratz, G., & Straub, R. H. (2014). The sympathetic nervous response in inflammation. Arthritis Research & Therapy, 16(6). doi:10.1186/s13075-014-0504-2
12. Skaar, E. P. (2010). The Battle for Iron between Bacterial Pathogens and Their Vertebrate Hosts. PLoS Pathogens, 6(8), e1000949. doi:10.1371/journal.ppat.1000949
13. Ravven, W. (2001) Signals from nervous system influence immune system, study shows. Research by the National Institutes of Health and the Medical Research Council of the UK.
Copyright InterClinical Laboratories 2020