Non-alcoholic Fatty Liver Disease NAFLD: An Unexpected Cause
InterClinical eNews February 2018, Issue 77
In this month’s issue, we look at recent research examining what might cause non-alcoholic fatty liver disease and in patients with none of the usual risk factors.
Liver Disease & Copper Deficiency
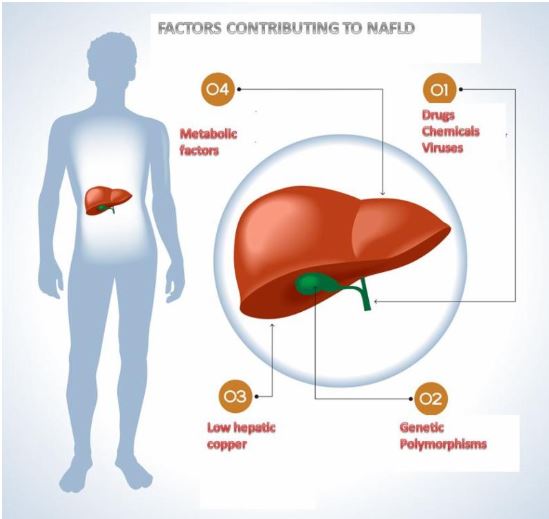
Non-Alcoholic Fatty Liver Disease (NAFLD) is a serious condition that is on the increase and has now become the most common liver disease in industrialised countries. A diagnosis of NAFLD involves a tissue biopsy or medical imaging. The factors leading to the development of NAFLD are multifactorial, such as metabolic, genetic, infectious agents, and exposure to certain drugs and chemicals.
More recently, dietary copper deficiency has also been implicated in the development of NAFLD. Copper is an essential trace element integral to several antiinflammatory hepatic enzymes, including copper-zinc superoxide dismutase, metallopeptidase, and metallothionein. HTMA is an excellent test for evaluating copper levels in the tissue. When interpreting an HTMA (Hair Tissue Mineral Analysis), it is important to look at the ratios of other minerals to copper, such as Zn/Cu, S/Cu, and Cu/Mo.
The results showed low hepatic copper was independently and negatively associated with moderate to severe steatosis but only in patients without MetS. P <0.001.
Metabolic Syndrome: A Predisposing Factor for Fatty Liver Disease
Widely accepted predisposing factors such as high blood pressure, high blood sugar, high serum triglycerides and low levels of high-density lipoprotein, collectively called Metabolic Syndrome. To investigate the role of other possible agents, this large-scale study comprising 174 adults caucasian adults sought to evaluate the role of hepatic copper and genetic polymorphism (PNPLA3) in non-alcoholic fatty liver disease (NAFLD) in patients with or without Metabolic Syndrome (MetS).
The participants underwent liver biopsy, and the percentage of steatosis was calculated. Hepatic copper levels were also measured by spectroscopy. In recent years, a substantial number of people have presented with NAFLD symptoms. Similarly, liver fibrosis was significantly more common in NAFLD participants with low copper, but these experimental results show that there are other pathways.
MetS P <0. 001 The mechanism by which low copper leads to steatosis development is currently poorly understood. However, some clues are emerging as patients with low copper tend to have elevated iron concentrations, a higher prevalence of siderosis and decreased levels of the hepatic iron transporter hepatic ferroportin mRNA.
Genetic polymorphism (PNPLA3)
Low hepatic copper and the genetic polymorphism (PNPLA3) are emerging as independent contenders for the development of NAFLD, especially in people with normal body weight and no signs of metabolic syndrome.
The PNPLA3 gene provides instructions for making a protein called adiponutrin, which is found in fat cells (adipocytes) and liver cells (hepatocytes). The liver is a part of the digestive system that helps break down food, store energy, and remove waste products, including toxins.
NCBI Gene Summary for PNPLA3 Gene – The protein encoded by this gene is a triacylglycerol lipase that mediates triacylglycerol hydrolysis in adipocytes. The encoded protein, which appears to be membrane-bound, may be involved in the balance of energy usage/storage in adipocytes.
GeneCards Summary for PNPLA3 Gene (Patatin Like Phospholipase Domain Containing 3) is a Protein Coding gene. Diseases associated with PNPLA3 include Liver Disease and Fatty Liver Disease 1. Among its related pathways are Glycerophospholipid biosynthesis and Metabolism. Gene Ontology (GO) annotations related to this gene include phospholipase A2 activity and mono-olein transacylation activity. An important paralog of this gene is PNPLA2. (Reference link)
REFERENCE
- Stättermayer AF, Traussnigg S, Aigner E, Kienbacher C, Huber-Schönauer U, Steindl-Munda P, Stadlmayr A, Wrba F, Trauner M, Datz C, Ferenci P. Low hepatic copper content and PNPLA3 polymorphism in non-alcoholic fatty liver disease in patients without metabolic syndrome. Journal of Trace Elements in Medicine and Biology. 2017;39:100-7.
Copyright InterClinical Laboratories 2018, 2020, 2024
No Comments
Sorry, the comment form is closed at this time.