Sodium – Mastering Minerals Series 1

In this article we look at the latest research on sodium, including storage, and an individual’s ability to absorb it and utilise it independent of intake.
Characteristics of sodium
InterClinical eNews July, Issue 108
Sodium is the sixth most abundant element in the earth’s crust and the second most abundant element in seawater. An adult human body contains about 250g of sodium and any excess is naturally excreted by the body. About 85% of sodium is found in the blood and lymphatic fluid. It is an electrolyte, like potassium, calcium and magnesium; it regulates the electrical charges moving in and out of the cells of the body.
It is an essential element for human life, involved in the maintenance of normal cellular homeostasis and in the regulation of fluid and electrolyte balance and blood pressure. The presence of sodium ions is essential for the contraction of muscles, including that largest and most important muscle, the heart. It is a cellular activator and is important for the excitability of nerve cells and for the transport of nutrients and substrates through plasma membranes. It controls your taste, smell and tactile processes and is fundamental to the operation of signals to and from the brain. Without sufficient sodium your senses would be dulled and your nerves would not function.
Sodium and diet
In modern medicine there is a generally negative feeling about sodium. It is well known that excessive dietary sodium intake is associated with hypertension, heart disease, osteoporosis and more. On the other hand, one study revealed that the evidence of the benefit of sodium restriction in patients with heart failure was inconclusive. 12
Approximately 10-15% of the population are salt sensitive, meaning that they retain sodium whether they consume large or small amounts. Generally this is due to hyperactive adrenal gland function and a deficiency of key minerals which help protect the body from sodium build-up. 12 Additionally, there is some debate over the recommended intake of sodium. Some researchers suggest that current recommendations for daily sodium intake may be set too low. 1
It is well known that a diet high in sodium is associated with a higher risk of developing hypertension and cardiovascular disease. However, a meta-analysis of sodium studies and hypertension stated that there is an association between low sodium (<3g/day or >7g/day sodium chloride) and increased cardiovascular disease and mortality, irrespective of hypertension status. It was proposed that this must indicate that mechanisms unrelated to blood pressure might be at play. 4
This analysis defined a high sodium intake as more than 6 g per day (15 g sodium chloride), whereas low sodium intake was defined as less than 3 g per day (or >7g per day sodium chloride). Lower sodium levels were correlated with higher rates of heart attack, stroke and death in normotensive individuals. It concluded that ‘reducing sodium intake among those with hypertension and high sodium intake was important, but it did not support reducing sodium intake to low levels’ for those who were normotensive. 4
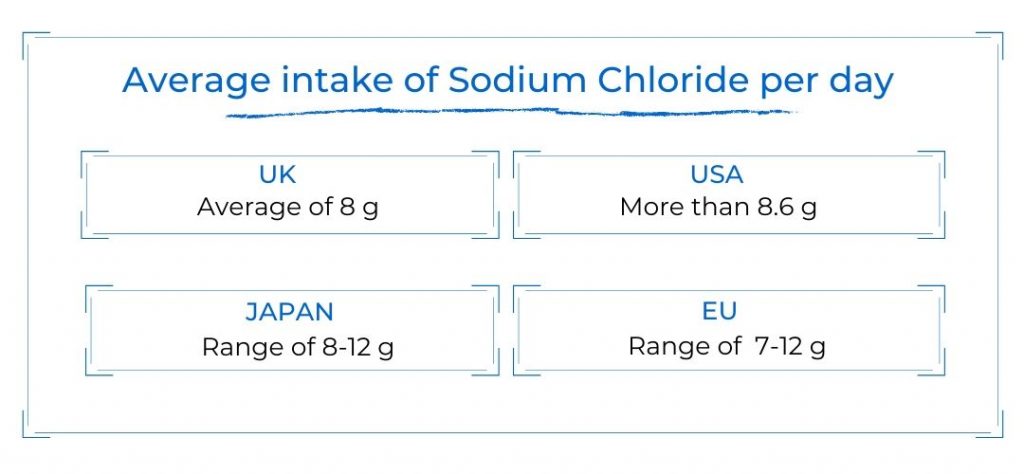
In Australia the National Health and Medical Research Council reviewed the recommended sodium intake in 2017. The NHMRC concluded that if the population were to reduce their average sodium intake to 2 g per day instead of the present average of 3.6 g, then desired blood pressure targets would more likely be achieved. 10
The update stated that ‘the upper limit was revised from the 2006 UL of 2.3 g/day (5.8 g sodium chloride) to ‘not determined’ reflecting the inability to identify a single point below which there is low risk of an increase in blood pressure.’ 10 For a comprehensive determination of risk, any discussion involving sodium intake must involve potassium, magnesium, calcium and other dietary factors.
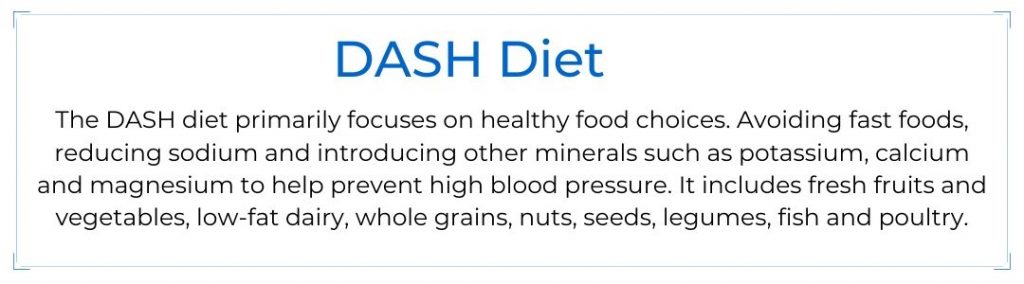
The DASH diet originated in the 1990s as a dietary intervention for treating hypertension. This diet was successful in lowering blood pressure, and implicated increased potassium intake. A diet high in sodium and low in potassium has been suspected in hypertension. Studies suggest that a diet high in potassium and fibre are associated with a reduced risk of hypertension. The combined effect of high sodium and low potassium on blood pressure seems greater than either one individually. 5
The DASH diet clinical trial examined whether sodium levels in the diet correlate with the energy intake from food. It found some conclusions to suggest that blood pressure rose more steeply with an increased sodium diet at lower energy intake than at higher energy intake. This suggests that sodium density may reflect the relationship with blood pressure better than an absolute sodium intake. 5
Differences in sodium retention can also be related to differences in kidney function and aldosterone levels. 6 Tissue sodium levels in the body are partly controlled by the hormone aldosterone, which is made by the adrenal glands. Sodium and also potassium levels indicate adrenal status. Low sodium and potassium relative to calcium and magnesium is an indicator of adrenal insufficiency. Conversely, high tissue levels of sodium and potassium relative to calcium and magnesium are indicative of high adrenal activity and associated with an increased stress response. 9
Sodium and health
Recent evidence suggests that gut microbiota contributes to the pathogenesis of hypertension. The gut microbiota is highly dynamic and mediates many physiological functions. These can be influenced by external factors. Interactions between dietary sodium and gut microbiota are just beginning to be explored. 5
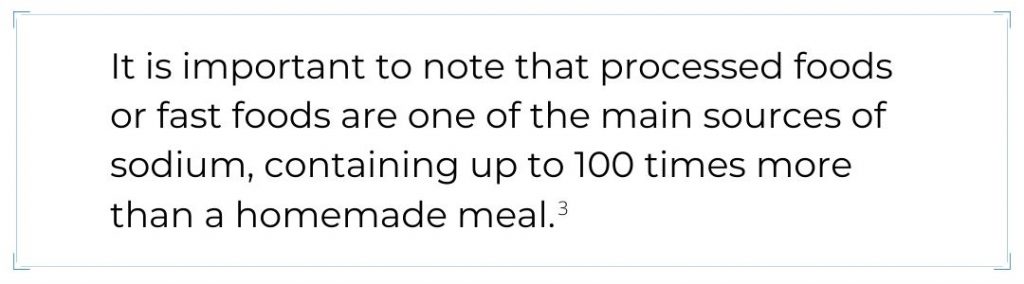
Research has found that a high sodium diet (above 6 g per day or 15g sodium chloride) significantly increased the Firmicutes/Bacterioidetes ratio in the gut microbiome, indicating gut dysbiosis. These and other changes in intestinal bacteria suggest that this could severely interfere with the symbiotic relationships among gut flora. This may be closely related to the development of hypertension. 5
There is growing evidence that excess sodium might be considered as a risk factor in autoimmune diseases such as multiple sclerosis. Several intestinal bacteria are affected by high sodium concentrations, particularly a Lactobacillus strain. One study found that a high sodium diet significantly reduces intestinal Lactobacillus murinus in mice. Depletion of Lactobacillus murinus by high sodium increased intestinal and systemic Th17 (CD4+ helper 17) levels. 7 Treatment with Lactobacillus prevented the sodium-induced increase of Th17 cells and prevented the exacerbation of experimental autoimmune encephalomyelitis, a rodent disorder similar to human multiple sclerosis. 3
High sodium concentrations induced the proliferation of Th17 cells coinciding with reduced indole-3-lactic acid, a bacterial fermentation compound produced by Lactobacilli. This has been implicated in the suppression of central nervous system autoimmunity. 3
Several studies have reported an association between dietary salt and cancer, especially gastric cancer. According to a review of the World Cancer Research Fund/American Institute for Cancer Research, the intake of salted foods and dietary salt are likely to increase the risk of gastric cancer. Japanese cohort studies have reported that dietary salt intake is positively associated with gastric cancer prevalence and mortality, while the frequency of the intake of salt-cured foods was associated with the risk of gastric cancer. 11
On the other hand hyponatraemia (abnormally low concentrations of sodium in the blood) is the most common electrolyte disorder seen in clinical practice. The consequences can range from minor symptoms to life-threatening complications. A diagnosis of hyponatraemia is based on the body’s fluid status. Hyperglycaemia, diuretics, adrenal insufficiency, hypothyroidism and some medications can cause sodium deficiency. 12
Adrenal insufficiency reduces the body’s ability to retain sodium. An extreme example is Addison’s disease where, due to an almost total lack of adrenal cortical hormone, there is a craving for salt. Often these individuals have high levels of calcium and magnesium which antagonise sodium which compounds the problem. 13
Determining Sodium status
Determining sodium status has generally been limited to urinary excretion testing. One of the methods used is a 24 hour urinary excretion test. However, a single 24 hour urine collection is an indicator of short term intake, and this can vary from day to day within individuals, and with foods consumed. Therefore this does not represent an individual’s usual long term daily sodium intake. 8
Multiple, 24 hour collections are necessary to assess salt intake and single spot urine collections are not a valuable tool. There is considerable day to day variation in 24 hour excretion even when dietary sodium intake is known and fixed over several weeks or months. Stability between sodium intake and sodium excretion follows weekly or even monthly rhythms of accumulation and secretion independent of dietary intake. The prevailing idea that excess dietary sodium leads to direct urinary excretion has been challenged by evidence of periodic sodium tissue storage. 3
Huge amounts of sodium can be stored in the body without changes in body weight, showing that sodium can be stored without water retention. So, it is necessary to establish new methods to accurately measure the sodium intake and storage in the body. 3 Alternative techniques such as non-invasive tissue sodium measurements such as Hair Tissue Mineral Analysis can provide more concise information.
InterClinical Comment
Although for some, elevated levels of sodium intake can have a detrimental impact on health, for others low levels can also create problems. For example, adrenal insufficiency, a prevalent issue today, can reduce the body’s ability to retain sodium. A hair tissue mineral analysis (HTMA) measurement of sodium is an excellent indicator of both underactive and overactive adrenal function. The ratio between sodium and potassium in a HTMA can provide a wealth of information, not only on sodium storage, but on our individual ability to absorb and utilise it.
A HTMA provides the critical measurement of long term sodium storage levels that a urine excretion test cannot. The discovery that sodium storage can be independent of dietary intake, and independent of fluid retention renders a urine excretion test less reliable. HTMA also determines an individual’s sodium storage ratio to each electrolyte. Determining our individual tissue sodium status in relation to potassium, magnesium and calcium is vitally important.
For more about InterClinical’s HTMA testing, visit here.
REFERENCES
1 Abraham W. T. 2008 Managing Hyponatremia in Heart Failure. US cardiology review 5(1):57-60
2 Strazzullo, P., & Leclercq, C. (2014). Sodium. Advances in Nutrition, 5(2), 188-190. doi:10.3945/an.113.005215
3 Haase, S., Wilck, N., Kleinewietfeld, M., Müller, D. N., & Linker, R. A. (2018). Sodium chloride triggers Th17 mediated autoimmunity. Journal of Neuroimmunology. doi:10.1016/j.jneuroim.2018.06.016
4 Mente, A., O’Donnell, M., Rangarajan, S., Dagenais, G., Lear, S., McQueen, M., … Yusuf, S. (2016). Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. The Lancet, 388(10043), 465–475. doi:10.1016/s0140-6736(16)30467-6
5 Svetkey, L. P., Sacks, F. M., Obarzanek, E., Vollmer, W. M., Appel, L. J., Lin, P.-H., Laws, R. L. (1999). The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-Sodium). Journal of the American Dietetic Association, 99(8), S96–S104. doi:10.1016/s0002-8223(99)00423-x
6 Yan, X., Jin, J., Su, X., Yin, X., Gao, J., Wang, X., Zhang, Q. (2020). Intestinal Flora Modulates Blood Pressure by Regulating the Synthesis of Intestinal-Derived Corticosterone in High Salt-Induced Hypertension. Circulation Research. doi:10.1161/circresaha.119.316394
7 Wilck, N., Matus, M. G., Kearney, S. M., Olesen, S. W., Forslund, K., Bartolomaeus, H., Müller, D. N. (2017). Salt-responsive gut commensal modulates TH17 axis and disease. Nature. doi:10.1038/nature24628
8 Cogswell, M. E., Loria, C. M., Terry, A. L., Zhao, L., Wang, C.-Y., Chen, T.-C., Appel, L. J. (2018).
9 Watts, D. Trace elements and other essential nutrients, 1995 Ch. 10, p 117-123
10 Nutrient Reference Values for Australia and New Zealand, Commonwealth of Australia 2016.
11 Dietary Reference Intakes for Japanese (2015) Ministry of Health, Labour and Welfare p.203.
12 Williams, D. M., Gallagher, M., Handley, J., & Stephens, J. W. (2016). The clinical management of hyponatraemia. Postgraduate Medical Journal, 92(1089), 407–411. doi:10.1136/postgradmedj-2015-133740
13 Watts, D. (1991) Sodium – Decrease or increase your intake? Trace Elements Newsletter 5 (1).
© InterClinical Laboratories Copyright 2020 at www.interclinical.com.au